Order Products:

Helpful Hints for using your
Lact-Aid® Nursing Trainer™ System NTS™
- Introduction
- Positioning the Lact-Aid® Nursing TrainerTM Unit
- Premature or Sick Babies
- Teaching Older or Reluctant Babies to Nurse
- Free Consulting Service
- Send us your suggestions
We always appreciate hearing from mothers about their experiences. It helps us improve the quality of our products and services to know if our instructions for use are clear and helpful. we’ve been listening to what they say from the very beginning. During our three-years of development and testing 1968 to 1971, and for 50+ years since we launched Lact-Aid® System mothers have helped us develop our product instructions and educational support literature. Every time we get ready to do a new printing, we review all the suggestions we receive. When we are complimented on how thorough and helpful our instructions are, we owe it to the moms who shared their ideas with us.
The information provided here is included as an Addendum to the instructions packed in every Lact-Aid® Nursing Trainer System. We hope it will help you and your baby enjoy a positive experience.
We welcome your comments and suggestions.
These suggestions about positioning have been found helpful by many mothers. The filled, assembled Nursing Trainer™ Unit may be used attached to the Neck Strap, or inserted into an optional lace pocket, which is available. (See your Lact-Aid Catalog/order form packed in your System, or refer to our online catalog.)
The Lact-Aid® Nursing TrainerTM Unit, when filled and assembled, consists of three (3) durable pieces, plus our own special disposable Nursing Bags.
|
|
Positioning the Nursing Trainer Unit

- Because of the unique flexible bag and other special design features, a great variety of flow rates can be achieved to accommodate different suckling abilities and various types of supplement.
- Raising it speeds the flow. Lowering it slows the flow.
- It may be used in an inverted (upside down) position by making a holder from an extra bag. (For a gravity-assisted flow for babies unable to suck due to cleft lip/palate, or other problem.) Refer to the booklet, Simple Ways to Evaluate and Adjust Flow, included with each Lact-Aid® Nursing Trainer™ System NTS™. (Soon this booklet will also be available to you in our Lact-Aid Online Library.)
Positioning the Nursing Tube & Breast Nipple:
-
Place the tip of the Nursing Tube about 1/4" past the end of the breast nipple. You may place a piece of tape over the tube at the edge of the areola, if desired.
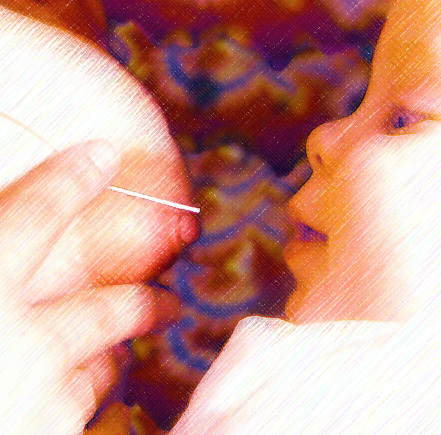
Positioning the Nursing Tube & Baby’s Mouth:
- The tube does not have to enter Baby’s mouth exactly at the center of Baby’s upper lip. The tube may enter slightly off center. (Imagine Baby’s mouth as the face of a clock. The center of the upper lip would be the 12:00 o’clock position. The tube may enter the mouth at 11:00 or 1:00.)

Positioning the Nursing Tube & Mother’s Hand:
- Support the breast from underneath with all your fingers (like a push-up bra) to keep the weight of the breast off Baby’s chin. Do NOT use a V Hold or a Cigarette Hold. Fingers tend to squeeze together and cause the Nursing Tube to curl. Failing to properly support the breast may cause Baby to pull his chin in and his head back. This can cause the nipple to slide partly or all the way out and leave only the tube in Baby's mouth. Some babies may clench their gums tightly to keep from losing hold of the nipple. Proper support prevents this problem.
Positioning Large Breasts & Mother’s Hand:
- Your hand may tire if you have large breasts. Make a support by folding a dry face wash cloth in half. Then roll it up, and fasten it into a roll with rubber bands or string. When you are ready to nurse, place the rolled up wash cloth under the breast, like a push-up pad. This will keep the weight of the breast off Baby’s chin, and you can give additional, but less tiring support under the breast as described above.
Avoiding Fatigue:
Premature and sick babies tire easily. They need to be fed in ways that help to conserve calories needed for growth and healing.
- Offer Lact-Aid System from the beginning of the feeding. Nursing the breast alone, then following with Lact-Aid System may overtire Baby. Many mothers do notice a more abundant milk supply mornings. Thus, for the first 1 or 2 feedings of the day, nursing first may be appropriate, then offer Lact-Aid System if needed.
- Short, frequent feedings. Feedings of 20 to 30 minutes' duration, offered 8 to 10 times a day may be overtiring. Try shorter feedings of 10 to 20 minutes, at more frequent intervals.
- Switch breasts often. Switch breasts about every 5 minutes, to stimulate and take advantage of multiple milk ejection reflexes. This reduces non-nutritive suckling that might otherwise occur during feeding times.
Excessive Crying:
Preemies, babies recovering from illness and babies gaining after having lost weight may begin crying a great deal, after having been quite passive previously. They also may seem to want to nurse almost constantly. Mothers often interpret this to mean Baby is hungry, or milk supply is low.
- Ask your doctor to confirm that Baby is gaining well and improving, and has no medical problem causing the excessive crying. In that case, crying likely indicates that Baby is expressing a need for a lot of close skin contact. This may be to help make up for separation and other discomfort Baby experienced due to the prematurity or illness.
- Try using a baby carrier that keeps Baby and Mother, (or Baby and Dad, Grandma, Grandpa, etc.) in close contact. When someone other than Mom is carrying baby like this, use of a pacifier can be calming, as well. Some moms find continuous nursing (non-nutritive suckling) between feedings tiring to the extent it inhibits milk ejection. In that case, consider pacifiers between feedings (while still continuing to provide lots of contact). After a few days, they may no longer be needed.
Teaching Older and Reluctant Babies to Nurse.
Sometimes, mothers attempting to relactate find that Baby is reluctant to take the breast. Efforts to go from bottle to breast abruptly are often unsuccessful. Baby has become accustomed to looking for the bottle as the signal to take the nipple. It may be necessary to actually re-teach Baby rooting behavior. This can be done easily, as follows:
- Plan on taking 3 or more days to make a gradual, gentle transition from bottle to breast.
- Use the NUK® Orthodontic Pacifier Nipple, which is now available in several sizes, including newborn. (Use the type intended for bottles without a collapsible bag. The bag allows liquid to flow too fast and may elicit a gag reflex, which Baby counteracts by gum clenching or tongue thrusting.)
- Have the filled, assembled Lact-Aid® Nursing Trainer™ Unit in position for each nursing.
- Try to use the same chair and location for every nursing during this time. Have a pillow available for your lap to help support Baby. The same setting will condition you, and the pillow helps relax your neck, shoulders, chest and arm muscles so blood and lactation hormones can circulate more freely and effectively.
- Hold Baby in breastfeeding position, with his/her cheek against your bare breast. Baby can begin to relearn that skin contact and your scent are part of feeding.
- The first efforts at nursing, you may have to show Baby the bottle, before inserting it into her mouth.
- Then, gradually move the bottle so it is next to your own bare breast and nipple. DO NOT try to offer the breast. Simply let Baby relax in a breastfeeding position in your arms, while nursing from the bottle.
- Talk softly, sing, caress Baby and make the experience of being in your arms as pleasant as possible for Baby and you. Repeat this for every feeding the first day.
- If you want to, try offering the breast once it is clear Baby is satisfied. Do not be disappointed if Baby does not mouth or suckle the breast. Keep in mind you are simply OFFERING the breast, at this point.
- The second day, show Baby the bottle, but then touch Baby’s cheek close to your breast so Baby must turn toward your bare breast to suckle the bottle nipple. Again, sing, caress, and do all you can to make it very pleasant for both you and Baby. If you offer the breast, do not be upset if Baby only mouths or plays with the nipple, or only nurses for a moment or two. Having the Lact-Aid® Nursing Trainer™ Unit in position will give Baby an immediate reward for suckling. Even if suckling is for just a moment, the idea is to make it a positive experience.
- For many babies, the third day is the turning point. The repeated bottle nursing in a breastfeeding style usually results in Baby automatically turning to root, find your nipple, and begin suckling when placed in breastfeeding position. Having your Lact-Aid® Nursing Trainer™ Unit filled and ready will reward Baby’s suckling and keep him on the breast.
- Once Baby has learned that breasts are a happy source of food, nursing usually progresses well. Keep in mind that this is simply a guide. For some mothers and babies, the progression of events from bottle to breastfeeding may take only a few feedings in a single day. For others it may take 4 to 10 days. The average is about three days for babies 4 to 6 months old. Making the transition from bottle to breast a gradual, loving process will take a great deal of pressure off Mom and Baby to perform. It avoids the pass or fail worries a mother might encounter if trying to make an abrupt change.
We really would love to hear from you. Sketches, photos, even videotapes are welcome, but cannot be returned. Please give your phone number so we may call you if we need to clarify details or obtain your permission to use photos. Names are kept confidential, and never revealed to others without your permission.
Lact-Aid International, Inc.
P.O. Box 2177, Ponte Vedra Beach, FL 32081