Order Products:

Relactation: One Alternative to Untimely Weaning
JANICE NAU, LPN
Reprinted from: KEEPING ABREAST JOURNAL. 2(3): 203-207, July-September 1977
When weaning is gradual and part of the normal progression of the nursing relationship, it can be just one of the many passages mothers and their children share in life, an experience filled with mutual satisfaction, development and emotional growth. Far too often, though, things happen which interfere with the natural progression of nursing and, as a result, many babies wean much sooner than their mothers expect. In my work as a lactation counselor, I have had the opportunity to learn first hand just how deeply disappointing such "untimely weaning" is for nursing mothers.
Sometimes there are situations in which the mother wants to or must wean her infant in the early weeks or months postpartum. The need to return to work is such a situation for some mothers. But even these weaning experiences can and should be planned for and carried out gradually and lovingly, so mother and infant can make the transition without disturbing the close relationship formed during nursing.
Most early weaning, though, is not a happy experience for mother or baby. Often, there are a number of factors causing untimely weaning such as poor breastfeeding information, getting off to a bad start in the hospital, regular use of supplemental bottle feedings, starting solids early and negative pressure from family, friends or medical professionals. These undermine the mother's confidence or reduce the amount of breast stimulation she receives. As a result, her milk supply gradually diminishes and, finally, her baby rejects the breast entirely.
The situation is common and until recently there was little one could do after the weaning to help mothers feel better about it. Many lactation counselors can tell of women who still get tears in their eyes when they confide to us their disappointment about an untimely weaning experience, even though their children are now grown.
For an increasing number of women, relactation is becoming an important alternative for coping with untimely weaning. Very simply, "relactation" is either rebuilding a very low milk supply or, in some cases, inducing lactation after it has completely stopped, in order to resume the nursing relationship. Techniques used can involve self-breast stimulation by massage or breast pump and re-teaching the baby to nurse at the breast. It almost always requires supplementing the baby until the supply is re-established.
Relactation isn't for everyone. Sometimes a mother inquires about it because of curiosity, her own guilt feelings or even pressure from others. Before a mother can decide if relactation is for her, she should consider a true analysis of both her and her husband's feelings about breastfeeding. In my work as a member of the Relactation Committee of La Leche League of Colorado, my major responsibility is to help the mother make a well-informed decision and then to support her in whatever she decides. I try to support the bond between the mother and her baby by helping her feel good about her mothering abilities, even if she does not resume breastfeeding.
I receive many calls about relactation, and for many different kinds of reasons. A typical call usually goes something like this:
MOTHER: Hello, my name is Molly. My friend gave me your name and number and said you might be able to help me bring my milk back in.
JAN: Can you tell me about it?
MOTHER: My baby, Anna, is 10 weeks old now. When she was just a couple of weeks old I saw the doctor and he said I should only nurse every 3-4 hours. I tried to do this but the baby was really fussy after 2 hours and she seemed to be hungry. I guess I didn't have enough milk because my doctor said to start supplementing after each feeding. Not long afterwards Anna wouldn't take the breast at all. She is doing fine now on the bottle but I really miss nursing.
JAN: The important thing is the mothering not the method of feeding your baby. You can be a good mother either way.
MOTHER: I know but I really miss the closeness I felt while I was breastfeeding. I enjoyed nursing. It was a special experience and I would like to do it again.
JAN: Do you have any milk now?
MOTHER: No, not really. Do you think you can help me?
The important thing is the mothering not the method of feeding your baby.
When a mother calls to tell me she is interested in breastfeeding, I ask her questions about several aspects of her experience, such as:
- Name and present age of baby.
- Baby's birth weight and present weight and, if applicable, any birth weight loss.
- Difficulties she is having.
- Solids or supplements and how much.
- Lactating now ... if so, how much?
- How long has it been since she last nursed?
- Are there any other children and did she nurse them?
- Is she on any medications (especially contraceptives or allergy medications?)
- What are her social activities and is she working outside the home?
- How does her husband feel about her relactating?
- How does her physician feel about her relactating? (She needs his full support.)
While discussing these questions I am careful to avoid giving advice. I feel the time for information and teaching can come later. If a great deal of advice is given at this point, it overwhelms the mother and is very frustrating for her.
I next explain the process of relactation. I found the Lact-Aid Nursing Trainer System method very helpful and most of the mothers I assist prefer to use it. (See Figure 1) Relactating takes time and patienc6 and there are many times when a mother may become discouraged. However, I assure the mother I will gladly provide encouragement and help.
Often questions come up about the length of time it will take for the milk to become reestablished. The milk supply cannot be predetermined. There are many variables that can affect this, such as how the breasts react to the stimulus, how the body adjusts to the hormonal changes which occur, the mother's own health and stamina, fatigue, family pressures and responsibilities and many other factors. It is known however, that the hormone level is the highest for three months following delivery and at that point it drops off sharply. The chances of reestablishing the milk supply are considerably better during this three-month period. The mother needs to be aware of all these factors so she will not become discouraged and wonder what is wrong with her or the baby if the milk supply seems to build more slowly than expected.
Figure 1 Lact-Aid NursingTrainer |
 |
Reducing anxiety and worry are especially important since they are well known to inhibit the let-down reflex. During this interval when the mother is discouraged she needs an extra amount of encouragement. She also needs reassurance that while her milk is coming in, she is establishing the closeness of the nursing relationship, which is so important.
BUILDING THE SUPPLY
The mother should nurse every two to three hours. At night, longer intervals are acceptable to help her get much needed rest since the relactating mother's milk supply can easily be inhibited by fatigue. Another factor that can slow down relactation is the tendency for the ovaries to resume ovulation when lactation is interrupted. Some mother's milk will be delayed in coming or it may reach a plateau or even decrease suddenly. The mother may have a menstrual period, slight spotting or feelings of premenstrual tension without menses. Within two to three days after this occurs her milk supply will probably build up at an even faster rate.
Often the let-down reflex is unstable at first. Remembering that the let-down is very easily conditioned to a routine stimulus can be very important in overcoming this problem. In addition to the conditioning process, it is important that the mother know the importance of adequate rest, a well balanced diet and good fluid intake. Warm support and help from her husband can also relieve this problem. if she is having extreme difficulty she may consult her physician about the use of oxytocin. (Available in a nasal spray, oxytocin stimulates the milk let-down reflex.) [Added note 1998. This is no longer available.]
In the past there has been some controversy over the methods of reestablishing an adequate milk supply. Many breastfeeding counselors have suggested gradually diluting supplemental formula thus "starving" the baby to produce more suckling, which in turn should build the milk supply. This method probably is useful when there are only a few ounces of supplement per day involved and only a moderate increase in the milk supply is needed. However, in relactation I feel the reduction of calories by diluting the formula does not stimulate milk production because the baby becomes weaker and, therefore, does not suck as effectively. This in turn does not produce the desired milk supply. By providing an adequate calorie intake, the baby remains strong and healthy with an adequate weight gain. This also puts more emphasis on the mother-child relationship and the mother has less of a tendency to become "milk oriented". She then can enjoy the baby and their relationship.
GETTING STARTED
While the mother is obtaining the Lact-Aid System the baby may need a gradual transition from the bottle to the breast. The mother can give the bottle next to the bare breast (Nuk nipples are the best because the shape promotes the same suckling action of mouth and jaw as the breast.) The skin contact and the baby's head turning restore the natural rooting behavior. Also she should not try to nurse the baby at the empty breast because doing so can negatively condition the baby by confusing him when there is no milk and he is hungry.
When the mother is ready to begin learning to use the device getting the tube situated just right can seem complicated at first. A few hints can save a lot of frustration. Here are some I have found helpful:
1. The best time to start is when the mother and baby feel the most rested and patient, usually in the morning.
2. Anticipate the baby's hunger and get ready before the baby is ready to eat. It is difficult to work with a frantic, hungry baby.
3. Position the tube so it extends slightly past the tip of the nipple. (Hair styling tape next to the areola helps to hold the tube in place.) When the baby is "latched on" the tube should extend down the center of the roof of his mouth toward the soft palate.
4. The baby should take four ounces of supplement in about 30-40 minutes. If it takes longer, test the Lact-Aid System by filling it with water and holding it upside down. There should be a steady, rapid dripping if the device is working properly. Refer to the instruction booklet for details on cleaning.
5. Some babies tend to tire more easily and need shorter, more frequent nursings.
6. Weak babies having difficulty sucking may be given slightly diluted supplement with physician's approval (to make the supplement flow easier one to two tablespoons of distilled water per four ounces of formula.)
ENCOURAGEMENT
After the excitement of finally getting the baby to nurse some mothers get the "one week blues." It seems to the mother that she has been nursing for ages and nothing has happened. The mother may be experiencing some feelings of fullness in her breasts. This is real encouragement indeed! Usually a few days later the mother will be able to express thick, sticky drops followed by milk several days later.
WEANING FROM THE LACT-AID SYSTEM
This is a very natural process if the mother is aware of the signs to watch for:
- The baby may spit up after each feeding.
- The baby will want to nurse less often; i.e., instead of every two to three hours he may want to go four hours between feedings.
- The baby may leave supplement in the bag after each feeding because the breast flows faster than the Lact-Aid System.
- The baby will have VERY wet diapers.
- The baby will have soft stools, more typical of breastfed infants.
- He will be gaining and thriving.
When these signs are occurring consistently, the mother can be assured that lactation is becoming well established and she can begin careful weaning from the Lact-Aid System.
- Slightly reduce the amount of supplement offered by how much is left in the bag. (See Instruction Book)
- Encourage the baby to empty both breasts before following with the Lact-Aid System.
- Offer the cooperative baby the breast between feedings as a pacifier.
- For the baby taking only an ounce per feeding, but who seems persistent in wanting the Lact-Aid System, introducing solids can be extremely helpful in establishing total breastfeeding with solids.
- Morning supplements are usually eliminated first.
- By the time the baby is five to six months old, mothers should be able to offer some of the supplement by cup, if any is needed.
There might be an occasional mother who may not be able to establish a fully adequate milk supply. However, with warm support, respect and kindness, she and her baby can certainly share many of the pleasures and rewards of nursing.
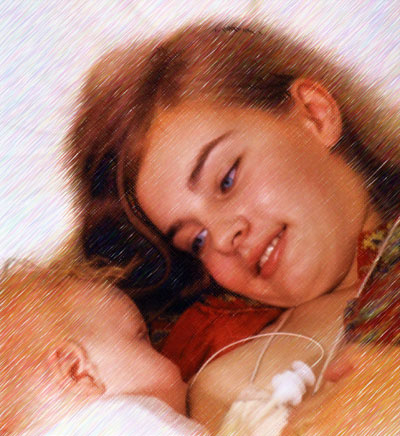
The return to breastfeeding can be a beautiful experience. As well as providing the best source of nutrition for the baby, nursing can be an expression of love and the nurturing of a strong bond between mother and baby.
BIBLIOGRAPHY
- Amsel P: The need to wean; as much for mother as for baby. RN 52-64 May 1976.
- Auerbach KG, et al: Breastfeeding the premature infant. Keep Abreast J 2(2): 98-121 Apr-June 1977.
- Avery, JL: Induced Lactation: A Guide for Counseling and Management. Denver, J J Avery, Inc. 1972.
- Brown RE: Breastfeeding in modern times. Am J Clin Nutr 26:556-562 May 1973.
- Jelliffe DB: Discussion (p. 68). In: CIBA: Breastfeeding and the Mother. Ciba Foundation Symp #45 (New series). Amsterdam, Elsevier 1976.
- Klaus MH, Kennell JH: Maternal-Infant Bonding. St. Louis, C V Mosby 1976.
- LLLI: The Womanly Art of Breastfeeding. Franklin Park IL, La Leche League 1958.
- Pasteels JL, Robyn C (Eds): Human Prolactin. New York, American Elsevier 1973.
- Pryor K: Nursing Your Baby. Revised Ed. New York, Harper & Row 1973.
- Raphael D: The Tender Gift: Breastfeeding. Englewood Cliffs NJ, Prentice-Hall 1973.
- Rees D: Sore nipples are a pain! Keep Abreast J 1(2): 137-144 April-June 1976.
- Schneour E: The Malnourished Mind. New York, Anchor Press/Doubleday 1974.
- Waletsky LR, Herman E: Relactation. AFP 14(2): Aug 1976.
At the time this article was published, Janice Nau, L.P.N., was a counselor for the Denver/Metro Area Relactation Committee of Colorado La Leche League. She frequently conducted workshops for La Leche League Leaders, childbirth educators and student nurses on relactation counseling. She currently resides in Anchorage, Alaska.
Disclaimer: The information presented here is for educational purposes only, and is not intended to provide or substitute for medical advice in any way. Anyone with a health question about breastfeeding, induced lactation, relactation, medications, adoption or for any other reason should discuss it with their physician.

